Cholesterol in the Blood
Facts about cholesterol
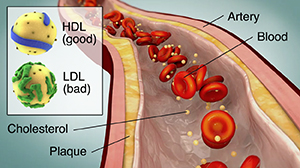
Cholesterol is a fat-like, waxy substance that can be found in all parts of your body. It helps your body make cell membranes, many hormones, and vitamin D. The cholesterol in your blood comes from 2 sources: the foods you eat and your liver. Cholesterol from food comes from animal sources such as meat and dairy. Your liver makes all the cholesterol your body needs.
Cholesterol and other fats are carried in your bloodstream as spherical particles called lipoproteins. The 2 most commonly known lipoproteins are low-density lipoproteins (LDL) and high-density lipoproteins (HDL).
|
What is LDL (low-density lipoprotein) cholesterol?
|
What is HDL (high-density lipoprotein) cholesterol?
|
|
LDL (bad) cholesterol is a type of fat in the blood that contains the most cholesterol. It can contribute to plaque buildup in the arteries (atherosclerosis). This is linked to higher risk for heart attack and stroke.
You want your LDL to be low. To help lower it:
-
Don't eat foods high in saturated fat and trans fat, such as red meat, fried foods, cheese, or butter. Eat a heart healthy diet that includes vegetables, fruits, whole grains, poultry, fish, nuts, and nontropical vegetable oils.
-
Exercise regularly
-
Stay at a healthy weight
-
Stop smoking, if you smoke
|
HDL (good) cholesterol helps to remove cholesterol from the blood. This keeps plaque from building up in your arteries.
You want your HDL to be as high as possible. Some people can raise HDL by:
-
Exercising for at least 30 minutes 5 times a week
-
Quitting smoking, if you smoke. Vaping also lowers HDL cholesterol.
-
Not eating saturated or trans fats
-
Losing weight, if needed. Losing even a small amount of weight (such as 5% of your body weight) is helpful.
Others may need medicine. Because raising HDL is complicated, you should work with your healthcare provider on a treatment plan.
|
Checking your blood cholesterol level
A cholesterol screening is an overall look at the fats in your blood. Screenings help find people at risk for heart disease. It is important to have what is called a full lipid profile to show the actual levels of each type of fat in your blood: LDL, HDL, triglycerides, and others. Talk with your healthcare provider about when to have this test.
Your cholesterol is checked with a simple blood test. Your healthcare provider will tell you if you need to not eat (fast) before the test. The results tell you how much cholesterol you have in your blood. Get checked as often as your healthcare provider suggests. Start keeping track of your cholesterol levels and other risk factors regularly at age 20. The American Heart Association (AHA) advises following up every 4 to 6 years. Check it earlier if you have an increased risk for either high cholesterol or heart disease. If you have diabetes or high cholesterol, you may need your blood tested as often as every 3 months. Discuss your numbers with your healthcare provider. You may need to be checked more often.
What is a healthy blood cholesterol level?
High blood cholesterol is a major risk factor for heart disease and stroke. You can lower your risk by getting more exercise, losing weight if you are overweight, quitting smoking, and eating a healthy diet. But blood cholesterol is very specific to each person. Your healthcare provider will determine your total cholesterol and LDL goals based on other risk factors. For that reason, a full lipid profile is an important part of your health history and important information for your healthcare provider to have.
What treatments are available for high cholesterol?
Medical treatment may include:
-
Changing risk factors. Some risk factors that can be changed include lack of exercise and poor eating habits.
-
Cholesterol-lowering medicines. Medicines are used to lower fats in the blood, particularly LDL cholesterol. Statins are a group of medicines that can do this. They include simvastatin, atorvastatin, rosuvastatin, and pravastatin. Other medicines that lower cholesterol levels are ezetimibe, PCSK9 inhibitors, bempedoic acid, bile acid sequestrants, such as colesevelam, cholestyramine, and colestipol, and nicotinic acid (niacin).
Statistics about cholesterol
High cholesterol is a risk for many Americans. Consider these statistics:
-
According to the CDC, about 86 million American adults age 20 and older have total blood cholesterol levels of 200 mg/dL and higher. Of those, about 25 million American adults have a level of 240 or above.
-
High cholesterol levels early in life may play a role in developing atherosclerosis as an adult.
-
According to the AHA, high blood cholesterol that runs in families will affect the future of an unknown but probably large number of children.
What are triglycerides?
Triglycerides are another class of fat found in the bloodstream. The bulk of your body's fat tissue is in the form of triglycerides.
Triglyceride levels and heart disease
The link between triglycerides and heart disease is being studied. But many people with high triglycerides also have other risk factors, like high LDL levels or low HDL levels.
What causes elevated triglyceride levels?
High triglyceride levels are linked with health conditions like diabetes, hypothyroidism, kidney disease, or liver disease. Dietary causes of high triglyceride levels may include drinking a lot of alcohol, eating foods containing saturated fat and trans fat, and eating lots of refined carbohydrates.
Online Medical Reviewer:
Brittany Poulson MDA RDN CD CDE
Online Medical Reviewer:
Heather M Trevino BSN RNC
Date Last Reviewed:
9/1/2025
© 2000-2025 The StayWell Company, LLC. All rights reserved. This information is not intended as a substitute for professional medical care. Always follow your healthcare professional's instructions.