Herpes Meningoencephalitis
What is herpes meningoencephalitis?
The meninges are the layers of thin tissue that cover your brain. Meningitis is when these tissues become inflamed or infected. The problem is called encephalitis when your brain becomes inflamed or infected. If both the meninges and the brain are infected, the condition is called meningoencephalitis .
Encephalitis involving herpes is a medical emergency. It needs to be diagnosed and treated right away. This disease is often fatal when it is not treated. Many people who survive it may have long-term problems afterward.
What causes herpes meningoencephalitis?
Meningitis and encephalitis may be caused by bacteria, fungi, or other types of germs. But many are caused by viruses. And many kinds of viruses can be to blame.
Herpes encephalitis is caused by the herpes simplex virus. Most are caused by herpes simplex virus type 1 (HSV1). This is the virus that also causes cold sores. The disease may also be caused by herpes virus type 2 (HSV2). This virus can be spread by sexual contact or from an infected mother to her baby during childbirth. HSV1 infection can also be sexually transmitted to the genital area. These viruses stay in the body throughout a person's life, even when they're not causing signs of infection.
Sometimes meningoencephalitis occurs during the initial infection with the herpes simplex virus. But most often it is caused by reactivation of the virus from an earlier infection.
What are the symptoms of herpes meningoencephalitis?
If you have viral meningitis, symptoms may include fever, light sensitivity, headache, and a stiff neck. If you have other symptoms, such as confusion, seizures, sleepiness, or a focal neurologic deficit—a nerve function problem that affects a specific area — your brain may also be affected. Your healthcare provider may diagnose it as meningoencephalitis.
These are possible symptoms of meningoencephalitis:
How is herpes meningoencephalitis diagnosed?
Your healthcare provider will ask about your medical history and symptoms. You may also need:
-
Neurological exam. Your provider will do a neurological exam to look for changes in motor and sensory function, vision, coordination, and balance. They will also check your mental status and look for changes in mood or behavior.
-
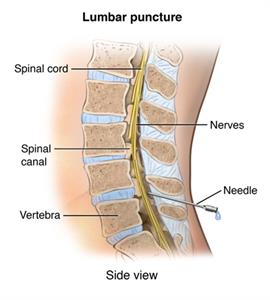
Spinal tap (lumbar puncture). In this procedure, your healthcare provider will remove a small amount of spinal fluid by a special needle inserted into the lower back. Cells and other substances in this fluid will be examined under a microscope in a lab and may help with the diagnosis.
-
CT scan or MRL scan. These tests create images of your brain.
-
Electroencephalogram (EEG). An EEG measures brain waves by placing electrodes onto your scalp.
-
Blood tests. Testing the blood helps identify infection.
If your healthcare providers think that a newborn has herpes encephalitis resulting from infection with HSV2 while passing through the birth canal, they may check samples of the baby's blood and spinal fluid.
How is herpes meningoencephalitis treated?
Treating the cause of your infection is the primary treatment. Since most cases of meningoencephalitis are caused by the herpes virus, the antiviral acyclovir is used to treat it. You may need to take this medicine through an intravenous (IV) line for 10 to 14 days. Your healthcare provider may also give you medicine to reduce swelling in the brain and to treat or prevent seizures.
Healthcare providers may treat babies with this disease with acyclovir for several weeks.
Depending on the severity of your infection, you may need to be treated in the hospital.
What are possible complications of herpes meningoencephalitis?
With treatment, most people with this disease start to get better within a day or two. They tend to recover fully within about a month. But without treatment, very serious complications can set in, including death.
Even with treatment, some people with severe cases may have long-term brain damage. They may have serious seizure disorders, memory problems, personality changes, trouble thinking, controlling their body, and hearing, seeing, or speaking. They may need to take medicines for a long time and may need long-term care.
What can I do to prevent herpes meningoencephalitis?
Not getting a herpes virus infection in the first place can help you prevent herpes meningoencephalitis. Ways to do this are:
-
Abstain from sex or have only one sex partner who has been tested for the virus and isn't infected.
-
Use a latex condom. This can reduce — but not entirely prevent — the risk of infection.
-
Don't kiss people with cold sore blisters. It's important to keep in mind that most people have already been infected with HSV1 by the time they're 20 years old. If you've already been infected, the virus goes dormant inside your body except during outbreaks. More than half of adults already carry HSV1 in their body.
Some pregnant women who have had genital herpes outbreaks may want to have their babies delivered by cesarean section. This may prevent meningoencephalitis in newborns.
When should I call my healthcare provider?
Treating herpes meningoencephalitis as soon as possible is essential. Call your healthcare provider or get medical care right away if you have:
If you already have herpes meningoencephalitis and are being treated, tell your healthcare providers if any of your symptoms get worse or if you develop any new symptoms. These could be signs that the infection is getting worse despite treatment.
Key points about herpes meningoencephalitis
-
Herpes meningoencephalitis is an infection of the brain and brain covering (meninges) caused by the herpes simplex virus. It is a medical emergency that needs treatment right away.
-
Symptoms can include headache, fever, changes in consciousness, confusion, neck stiffness, sensitivity to light, seizures, and changes in mood, personality, or behavior.
-
Treatment is with antiviral medicine. You may also need steroids or medicines to prevent seizures.
Next steps
Tips to help you get the most from a visit to your healthcare provider:
-
Know the reason for your visit and what you want to happen.
-
Before your visit, write down questions you want answered.
-
Bring someone with you to help you ask questions and remember what your provider tells you.
-
At the visit, write down the name of a new diagnosis, and any new medicines, treatments, or tests. Also write down any new instructions your provider gives you.
-
Know why a new medicine or treatment is prescribed, and how it will help you. Also know what the side effects are.
-
Ask if your condition can be treated in other ways.
-
Know why a test or procedure is recommended and what the results could mean.
-
Know what to expect if you do not take the medicine or have the test or procedure.
-
If you have a follow-up appointment, write down the date, time, and purpose for that visit.
-
Know how you can contact your healthcare provider if you have questions.