Acute Spinal Cord Injury (SCI)
What is an acute spinal cord injury?
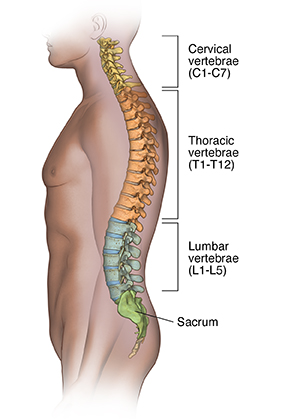
Your spine is made of many bones called vertebrae. Your spinal cord runs downward through a canal in the center of these bones. The spinal cord is a bundle of nerves that carries messages between the brain and the rest of the body. This is for movement and sensation.
Acute spinal cord injury (SCI) is a traumatic injury that bruises, partially, or completely tears the spinal cord. SCI is a common cause of permanent disability and death in children and adults.
What causes an acute SCI?
Many things can cause SCI. The more common injuries occur when the area of the spine or neck is bent or compressed, as in the following:
-
Falls
-
Motor vehicle accidents, such as cars, motorcycles, and being struck when walking
-
Sports injuries
-
Diving accidents
-
Trampoline accidents
-
Violence, such as gunshot or stab wounds
-
Infections that form a collection of pus (abscess) on the spinal cord
-
Birth injuries. These typically affect the spinal cord in the neck area.
Who is at risk for acute SCI?
Some people are at higher risk for SCI than others. Those at higher risk are people ages 16 to 30 or older than age 65. tThe majority of people who suffer SCIs are male. Non-Hispanic whites are at higher risk for SCI than any other ethnic group.
What are the symptoms of an acute SCI?
Symptoms of an acute SCI can vary widely. The location of the injury on the spinal cord determines what part of the body is affected. And how bad the symptoms are.
Your spine may be in shock right after a spinal cord injury. This causes loss or decrease in feeling, muscle movement, and reflexes. It will be easier for your healthcare provider to find out the extent of injuries as swelling eases.
Generally, the higher up the level of the injury is to the spinal cord, the more severe the symptoms. For example, an injury to the neck, the first and second vertebrae in the spinal column (C1, C2), or the midcervical vertebrae (C3, C4, and C5) affects the respiratory muscles and the ability to breathe. A lower injury, in the lumbar vertebrae, may affect nerve and muscle control to the bladder, bowel, and legs, and sexual function.
The extent of the damage to the spinal cord determines whether the injury is complete or incomplete.
-
A complete injury means that there is no movement or feeling below the level of the injury.
-
An incomplete injury means that there is still some degree of feeling or movement below the level of the injury.
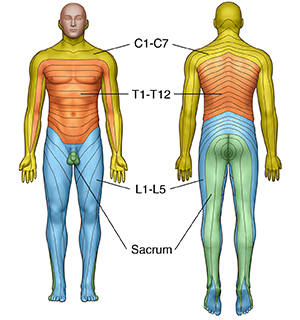 |
| Areas of sensation (dermatomes). |
These are the most common symptoms of acute spinal cord injuries:
-
Muscle weakness
-
Loss of voluntary muscle movement in the chest, arms, or legs
-
Breathing problems
-
Loss of feeling in the chest, arms, or legs
-
Loss of bowel and bladder function
The symptoms of SCI may look like other health conditions or problems.
How are acute SCIs diagnosed?
Acute SCI is a medical emergency. Emergency evaluation is needed anytime there is a suspected injury to the spinal cord.
The effects of an SCI may not be clear at first. A full health evaluation and tests are needed. During the exam, the healthcare provider will ask about your health history and how the injury occurred. A spinal cord injury can cause ongoing nerve problems. These will need more medical follow-up. Sometimes, surgery is needed to stabilize the spinal cord after acute SCI.
Diagnostic tests may include:
-
Blood tests
-
X-ray. This test uses invisible electromagnetic energy beams to make images of internal tissues, bones, and organs onto film.
-
CT scan. An imaging test that uses X-rays and computer technology to make detailed images of the body. A CT scan shows images of any part of the body. This includes the bones, muscles, fat, and organs. CT scans are more detailed than general X-rays.
-
MRI scan. This test uses large magnets, radio waves, and a computer to make detailed images of organs and structures within the body. This is done without using X-rays.
How is an acute SCI treated?
SCI needs emergency medical attention on the scene of the accident or injury. Your head and neck will be immobilized to prevent movement after an injury. This may be very hard when you are frightened after a serious accident.
There is currently no way to repair a damaged or bruised spinal cord. But researchers are actively seeking ways to stimulate spinal cord regeneration. The severity of the SCI and the location determines if the SCI is mild, severe, or fatal.
You may need surgery to assess the injured spinal cord and stabilize fractured backbones. Surgery can also release the pressure from the injured area. You may need surgery to manage any other injuries that may have been a result of the accident. Your treatment may include:
-
Observation and management in the intensive care unit
-
Medicines, such as corticosteroids, to help decrease the swelling in the spinal cord
-
Breathing machine (mechanical ventilator), to help you breathe
-
Bladder catheter, a tube that is placed into the bladder. This helps to drain urine into a collection bag.
-
Feeding tube. This is put through the nostril to the stomach. Or it's put directly through the abdomen (belly) into the stomach. The tube provides extra nutrition and calories.
Recovery from a SCI often needs a long-term stay in a hospital and rehabilitation. You will be cared for by a team of healthcare providers from many fields. The team will include nurses, therapists (physical, occupational, or speech), and other specialists. They will work to control your pain and to keep track of your heart function, blood pressure, body temperature, nutritional status, and bladder and bowel function. They will also attempt to control involuntary muscle shaking (spasticity).
Can acute SCIs be prevented?
There is no sure way to prevent SCI, but there are many steps you can take that might lower your risk. These include:
-
Don’t drive when you are under the influence of alcohol or drugs.
-
Always wear a seat belt while in a vehicle.
-
Take precautions to prevent falls around your home.
-
Keep firearms unloaded and locked away.
-
Wear a helmet when riding a motorcycle or taking part in any sports or activities that may result in head injury. These include bike riding, skiing, hockey, and football.
-
Don't dive into shallow water
Living with an acute SCIs
Physical therapy will likely be a very important part of your rehabilitation. In this treatment, specialists will work with you to prevent muscle wasting and shortening (contractures), and to help you retrain other muscles to aid in mobility and movement. Another type of therapy is occupational therapy. It helps you learn new ways of doing everyday tasks in spite of your new physical limitations.
A traumatic event that results in a SCI is devastating to both you and your family. The healthcare team will help educate your family after your hospital stay and rehabilitation on how to help care for you at home. They will also help you understand the specific problems that need medical attention right away.
You will need frequent medical evaluations and testing after your hospital stay and rehabilitation to keep track of your progress.
It’s important to focus on maximizing your capabilities at home and in the community.
You may feel sad or depressed after your injury. If this happens to you or a loved one, your healthcare provider may recommend that you see a mental health professional. Antidepressants and talk therapy (psychotherapy) can help treat depression.
When should I call my healthcare provider?
Depending on the severity of the injury, some people might recover some of their lost function, but others might continue to have long-term problems. Be sure to talk with your healthcare provider about when you would need to call them.
Your healthcare provider will likely advise you to call them if any problems you are having become worse, including weakness, numbness or other changes in sensation, or changes in bladder or bowel control.
People who have serious long-term effects from a spinal cord injury can also develop a number of other complications. Your healthcare provider might advise you to call them if you have problems, such as:
-
Skin sores or infections
-
Trouble breathing
-
Fever, cough, or other signs of infection
-
Severe headache
-
Not urinating regularly or having severe diarrhea or constipation
-
Severe muscle cramps or spasms
-
Increasing pain
-
Sudden blood pressure changes
Key points about acute SCIs
-
An acute spinal cord injury is caused by trauma to the spinal cord. It's a medical emergency that needs to be treated right away.
-
The severity of symptoms (such as weakness, paralysis, and loss of feeling) depends on how badly the spinal cord is damaged and where on the cord the injury occurs. Damage to the cord in the middle of the back might affect only the legs, whereas damage to the spinal cord in the neck might also affect the arms and even the breathing muscles.
-
Treatment might include surgery, medicine, and other treatments as needed. Some people might recover some function over time, but others might continue to have long-term problems. Physical and occupational therapy can help you adapt to new ways of doing things.
Next steps
Tips to help you get the most from a visit to your healthcare provider:
-
Know the reason for your visit and what you want to happen.
-
Before your visit, write down questions you want answered.
-
Bring someone with you to help you ask questions and remember what your provider tells you.
-
At the visit, write down the name of a new diagnosis, and any new medicines, treatments, or tests. Also write down any new instructions your provider gives you.
-
Know why a new medicine or treatment is prescribed, and how it will help you. Also know what the side effects are.
-
Ask if your condition can be treated in other ways.
-
Know why a test or procedure is recommended and what the results could mean.
-
Know what to expect if you do not take the medicine or have the test or procedure.
-
If you have a follow-up appointment, write down the date, time, and purpose for that visit.
-
Know how you can contact your provider if you have questions.