Amyotrophic Lateral Sclerosis (ALS)
What is ALS?
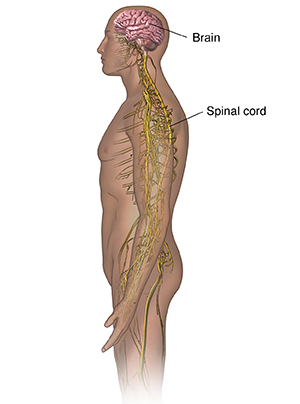
Amyotrophic lateral sclerosis (ALS) is a fatal type of motor neuron disease. It causes progressive degeneration of nerve cells in the spinal cord and brain. It's often called Lou Gehrig disease, named for a famous baseball player who died from the disease. ALS is one of the most devastating types of disorders that affect nerve and muscle function.
ALS doesn't affect the senses (such as seeing or hearing). It also usually doesn't affect mental functioning. It isn't contagious. You can't catch ALS from others. Currently, there is no cure for this disease.
ALS most often affects people between ages 40 and 70. But it can occur at a younger age. It affects people of all races and ethnic groups.
There are two main types of ALS:
-
Sporadic. This is the most common form of ALS in the United States, making up 90% of cases. These cases occur randomly, without any known genetic cause or family history of ALS.
-
Familial. This is an inherited form of ALS that affects a small amount of people. But many recent genetic discoveries suggest hereditary forms of ALS are more common than previously thought.
What causes ALS?
Experts don't know the cause of ALS. More recently, genetic causes are being seen as increasingly important. Research is also looking into possible environmental causes of ALS.
What are the symptoms of ALS?
With ALS, you may first have weakness in a limb that occurs over a few days or, more often, a few weeks. Then a few weeks or months later, weakness develops in another limb. For other people, the first sign of a problem may be slurred speech or trouble swallowing.
As ALS progresses, more and more symptoms are noticed. The most common symptoms of ALS include:
-
Twitching and cramping of muscles, especially those in the hands and feet.
-
Loss of motor control in the hands and arms.
-
Trouble using arms and legs.
-
Tripping and falling.
-
Dropping things.
-
Lasting severe tiredness (fatigue).
-
Uncontrollable periods of laughing or crying.
-
Slurred or thick speech and trouble projecting the voice.
As the disease progresses, symptoms may include:
-
Trouble breathing.
-
Trouble swallowing.
-
Paralysis.
Some of these symptoms may be caused by other health problems. Always see your doctor for a diagnosis.
How is ALS diagnosed?
There is no specific test to diagnose ALS. Your doctor will consider your health history and symptoms. You will also have tests to rule out other conditions. Tests may include:
-
Lab tests. These include blood and urine studies.
-
Electrodiagnostic tests, such as electromyography and nerve conduction study. These studies evaluate and diagnose disorders of the nerves, muscles, and motor neurons. Your doctor inserts electrodes into the muscle or places them on the skin overlying a muscle, a nerve, or muscle group to record electrical activity and muscle responses.
-
MRI scan. This procedure uses large magnets, radio waves, and a computer to make detailed images of organs and structures in the body without the use of X-ray.
-
Genetic tests. These can check for the known hereditary causes of ALS.
In some cases, other tests may be needed due to atypical features of ALS, such as:
-
Muscle or nerve biopsy. In this procedure, your doctor removes a sample of tissue or cells from the body and examines it under a microscope.
-
Spinal tap (lumbar puncture). In this test, your doctor places a special needle into the lower back, into the area around the spinal cord. There they can measure the pressure in the spinal canal and brain. Your doctor will remove a small amount of cerebrospinal fluid (CSF) and test it for an infection or other problems. CSF is the fluid that bathes the brain and spinal cord.
How is ALS treated?
For most people with ALS, the main treatment may include managing symptoms. This may include physical, occupational, speech, respiratory, and nutritional therapies. Some medicines and heat or whirlpool therapy may help ease muscle cramping. Exercise in moderation may help maintain muscle strength and function.
There is no cure and no proven treatment for ALS. But the FDA has approved the medicines riluzole, edavarone, and tofersen.
These medicines may improve short-term survival or slow physical decline in people with ALS. Tofersen is only helpful for people with a specific genetic form of ALS.
Coping with ALS and managing your symptoms is challenging for you, your caregivers, and your care team. But it’s important to know that there are many community resources available for support and assistance.
Researchers are conducting studies to better understand genes that may cause the disease. They are looking at the mechanisms that can set off motor neurons to degenerate in ALS. And they're also looking at ways to stop the progress leading to cell death.
What are possible complications of ALS?
There is no cure for ALS. For most people, the disease will progress over 3 to 5 years, making voluntary movements of arms and legs impossible. In other people, the disease can rapidly get worse over a few months. Or it can have a very slow course over many years. Each person is affected differently. In time, you will need help with personal care, eating, and mobility. Movement of the diaphragm for breathing is also impaired. You may need a machine (ventilator) for breathing. Most people with ALS die from respiratory failure. People with ALS are at risk of other complications because of the loss of mobility. These include pressure injuries. They are also at risk of losing weight from loss of muscle mass, as well as malnourishment. Muscle stiffness develops from spasticity. This can make mobility worse and cause discomfort. Some people will drool because of lower facial weakness.
Living with ALS
Over time, ALS will lead to disability and death. Your ability to move and breathe independently will be affected, but your intelligence and ability to think is usually not. You and your family will work closely with your doctor to manage symptoms as they develop. Using medicines may prolong your life by a few months, particularly if you have trouble swallowing. Discuss ways to make living spaces more accessible and the use of mobility devices and wheelchairs. It’s very important to talk about end-of-life decisions with your loved ones.
Support groups, such as the ALS Association, may help you cope with the disease. Talk with your doctor about how you feel about a feeding tube and breathing machine.
Many families find that professional counseling helps them develop coping strategies. Emotional support can also help people manage the complex emotional and physical challenges of this disease. Ask your doctor for resources.
When to contact your doctor
It's important to tell your doctor about new symptoms so they can advise you on therapies and community resources. Most importantly, contact your doctor if you start to have trouble breathing.
Key points about ALS
-
ALS is a fatal motor neuron disease. It causes progressive degeneration of nerve cells in the spinal cord and brain.
-
ALS affects voluntary control of arms and legs and leads to trouble breathing.
-
ALS doesn't affect intelligence, thinking, seeing, or hearing.
-
There is no known cure for ALS.
-
Treatment of ALS focuses on managing or reducing symptoms as much as possible.
Next steps
Here are some tips to help you get the most from a visit to your doctor:
-
Know the reason for your visit and what you want to happen.
-
Before your visit, write down questions you want answered.
-
Bring someone with you to help you ask questions and remember what your doctor tells you.
-
At the visit, write down the name of a new diagnosis, and any new medicines, treatments, or tests. Also write down any new instructions your doctor gives you.
-
Know why a new medicine or treatment is prescribed, and how it will help you. Also know what the side effects are and when they should be reported.
-
Ask if your condition can be treated in other ways.
-
Know why a test or procedure is recommended and what the results could mean.
-
Know what to expect if you don't take the medicine or have the test or procedure.
-
If you have a follow-up appointment, write down the date, time, and purpose for that visit.
-
Know how you can contact your doctor if you have questions, especially after office hours or on weekends.