Bell's Palsy
What is Bell's palsy?
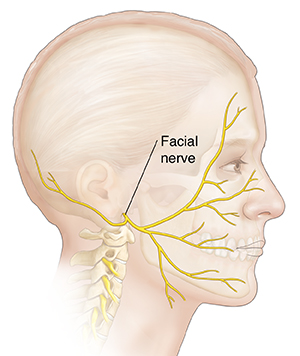
Bell's palsy is weakness or paralysis of the muscles of the face. It begins suddenly and can get worse over 48 hours. This condition results from damage to the facial nerve (the 7th cranial nerve). Pain and discomfort usually happen on one side of the face or head.
Bell's palsy can affect anyone at any age. But it's less common before age 15 and after age 60. It occurs most often with pregnancy, diabetes, influenza, a cold, or another upper respiratory ailment.
Bell's palsy is not considered long-lasting. But in rare cases, it doesn't go away. There's no known cure for Bell's palsy. But recovery usually begins 2 weeks to 6 months from the start of the symptoms. Most people with Bell's palsy recover full facial strength and expression.
What causes Bell's palsy?
The cause of Bell's palsy is not known. It may be due to the body's immune system causing inflammation in the facial nerve. Bell's palsy is sometimes linked to other conditions, including:
What are the symptoms of Bell's palsy?
The most common symptoms of Bell's palsy are:
-
Disordered movement of the muscles that control facial expressions, such as smiling, squinting, blinking, or closing the eyelid.
-
Headache.
-
Tearing.
-
Drooling.
-
Loss of the sense of taste on the front 2/3 of the tongue.
-
Hypersensitivity to sound in the affected ear (hyperacusis).
-
Inability to close the eye on the affected side of the face.
The symptoms of Bell's palsy may look like other health problems, such as Guillain-Barré syndrome, myasthenia, and multiple sclerosis. Always see your doctor for a diagnosis.
How is Bell's palsy diagnosed?
Your doctor can usually diagnose Bell's palsy by looking at your symptoms. There are no specific tests used to diagnose Bell's palsy. But your doctor may order tests to rule out other conditions that can cause similar symptoms. They may also order tests to find out the extent of nerve involvement or damage. These tests may include:
-
Electromyography to determine the extent of the nerve involvement.
-
Blood tests to determine if another condition is present, such as diabetes or Lyme disease.
-
MRI or CT scan to find out if there is a structural cause for your symptoms.
How is Bell's palsy treated?
If a cause for Bell's palsy is found, such as infection, that cause will be treated. Otherwise, your symptoms are treated as needed.
You'll need to protect your eye from drying at night or while working at a computer. Eye care may include eye drops during the day, ointment at bedtime, or a moisture chamber at night. This helps protect the cornea from being scratched. This is very important to manage Bell's palsy.
Your doctor will prescribe other treatment for your condition based on how bad your symptoms are and your health history. Other treatment choices include:
-
Steroids to reduce inflammation.
-
Antiviral medicine, such as acyclovir.
-
Analgesics or moist heat to relieve pain.
-
Physical therapy to stimulate the facial nerve.
Some people may choose to use alternative therapies to help treat Bell's palsy. But there is no proof they make a difference in recovery. Such treatment may include:
What are possible complications of Bell's palsy?
Bell's palsy usually resolves in time and causes no long-term problems. But during the illness, most people are unable to close their eye on the affected side of their face. So it's important to protect the eye from drying at night or while working at a computer.
A small number of people continue to have some weakness of the face. They may need surgery if the weakness greatly affects the eyelids. Others may have abnormal uncontrolled movements of the face (spasms) because of abnormal nerve repair.
Living with Bell's palsy
It's important to take medicines as directed. And be sure to protect the affected eye from drying. You can use eye drops during the day and ointment at bedtime to protect the cornea from scratching.
When to contact your doctor
Bell's palsy usually starts to improve in 2 weeks. But it may take 3 to 6 months to return to normal. Contact your doctor if you don't get better, you have new symptoms, or your symptoms get worse.
Key points about Bell's palsy
-
Bell's palsy is weakness or paralysis of the muscles of the face. It usually goes away on its own and causes no problems.
-
The cause of Bell's palsy is not known. But it's thought to be caused by inflammation affecting the body’s immune system. It's linked to other conditions, such as diabetes.
-
Symptoms of facial weakness or paralysis get worse over the first few days and start to improve in about 2 weeks.
-
It can take 3 to 6 months to fully go away.
-
Medicine and eye care are important in treating Bell's palsy.
Next steps
Tips to help you get the most from a visit to your doctor:
-
Know the reason for your visit and what you want to happen.
-
Before your visit, write down questions you want answered.
-
Bring someone with you to help you ask questions and remember what your doctor tells you.
-
At the visit, write down the name of a new diagnosis, and any new medicines, treatments, or tests. Also write down any new instructions your doctor gives you
-
Know why a new medicine or treatment is prescribed, and how it will help you. Also know what the side effects are.
-
Ask if your condition can be treated in other ways.
-
Know why a test or procedure is recommended and what the results could mean.
-
Know what to expect if you do not take the medicine or have the test or procedure.
-
If you have a follow-up appointment, write down the date, time, and purpose for that visit.
-
Know how you can contact your doctor if you have questions, especially after office hours or on weekends.