Lumbar Disk Disease (Herniated Disk)
What is lumbar disk disease?
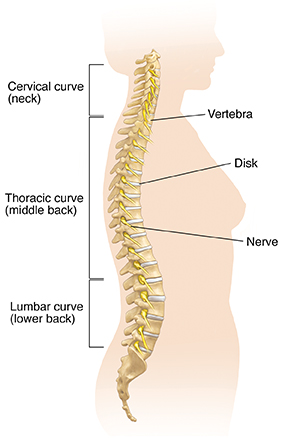
The vertebral column, or backbone, is made up of 33 vertebrae that are separated by spongy disks. The spine is divided into 4 areas:
-
Cervical spine. The first 7 vertebrae, located in the neck
-
Thoracic spine. The next 12 vertebrae, located in the chest area
-
Lumbar spine. The next 5 vertebrae, located in the lower back
-
Sacral spine. The lowest 5 vertebrae, located below the waist, including the 4 vertebrae that make up the tailbone (coccyx)
The lumbar spine consists of 5 bony segments in the lower back area, which is where lumbar disk disease occurs.
-
Bulging disk. With age, the intervertebral disk may lose fluid and become dried out. As this happens, the spongy disk (which is located between the bony parts of the spine and acts as a “shock absorber”) becomes compressed. This may lead to the breakdown of the tough outer ring. This lets the nucleus, or the inside of the ring, bulge out. This is called a bulging disk.
-
Ruptured or herniated disk. As the disk continues to break down, or with continued stress on the spine, the inner nucleus pulposus may actually rupture out from the annulus. This is a ruptured, or herniated, disk. The fragments of disk material can then press on the nerve roots located just behind the disk space. This can cause pain, weakness, numbness, or changes in sensation.
Most disk herniations happen in the lower lumbar spine, especially between the fourth and fifth lumbar vertebrae and between the fifth lumbar vertebra and the first sacral vertebra (the L4-L5 and L5-S1 levels).
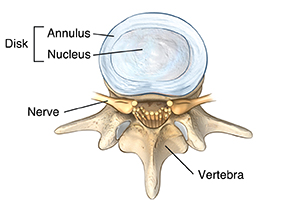 |
| Top view of normal lumbar disk. |
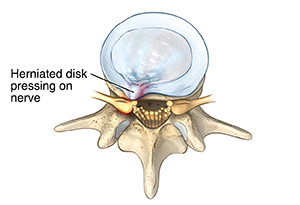 |
| Top view of herniated lumbar disk. |
What causes lumbar disk disease?
Lumbar disk disease is caused by a change in the structure of the normal disk. Most of the time, disk disease happens as a result of aging and the normal breakdown that occurs within the disk. Sometimes, severe injury can cause a normal disk to herniate. Injury may also cause an already herniated disk to worsen.
Who is at risk for lumbar disk disease?
Although age is the most common risk, physical inactivity can cause weak back and abdominal muscles, which may not support the spine properly. Back injuries also increase when people who are normally not physically active participate in overly strenuous activities. Jobs that require heavy lifting and twisting of the spine can also cause back injuries.
What are the symptoms of lumbar disk disease?
The symptoms of lumbar disk disease vary depending on where the disk has herniated and what nerve root it is pushing on. These are the most common symptoms of lumbar disk disease:
-
Intermittent or continuous back pain. This may be made worse by movement, coughing, sneezing, or standing for long periods of time.
-
Spasm of the back muscles
-
Sciatica. This is pain that starts near the back or buttock and travels down the leg to the calf or into the foot.
-
Muscle weakness in the legs
-
Numbness in the leg or foot
-
Decreased reflexes at the knee or ankle
-
Changes in bladder or bowel function
The symptoms of lumbar disk disease may look like other health conditions. Always see your healthcare provider for a diagnosis.
How is lumbar disk disease diagnosed?
In addition to a complete medical history and physical exam, you may have one or more of the following tests:
-
X-ray. This test uses invisible electromagnetic energy beams to produce images of internal tissues, bones, and organs onto film.
-
MRI. This procedure uses a combination of large magnets, radiofrequencies, and a computer to produce detailed images of organs and structures within the body without the use of X-rays.
-
Myelogram. This procedure uses dye injected into the spinal canal to make the structure clearly visible on X-rays.
-
CT scan. This imaging procedure uses X-rays and computer technology to make detailed images of any part of the body, including the bones, muscles, fat, and organs. CT scans are more detailed than general X-rays.
-
Electromyography (EMG). This test measures muscle response or electrical activity in response to a nerve’s stimulation of the muscle. This tests to see if there is any associated nerve damage.
-
Discogram. This procedure uses a needle that is inserted into the disk under X-ray guidance.
How is lumbar disk disease treated?
Typically, conservative therapy is the first line of treatment to manage lumbar disk disease. This may include a mix of the following:
-
Bed rest
-
Education on proper body mechanics (to help decrease the chance of worsening pain or damage to the disk)
-
Physical therapy, which may include ultrasound, massage, conditioning, and exercise programs
-
Weight control
-
Use of a lumbosacral back support
-
Medicine to control pain and relax muscles
If these measures fail, you may need surgery to remove the herniated disk. Surgery is done under general anesthesia. Your surgeon will make an incision in your lower back over the area where the disk is herniated. Some bone from the back of the spine may be removed to gain access to the disk. Your surgeon will remove the herniated part of the disk and any extra loose pieces from the disk space.
After surgery, you may be restricted from activity for several weeks while you heal to prevent another disk herniation. Your surgeon will discuss any restrictions with you.
What are possible complications of lumbar disk disease?
Lumbar disk disease can cause back and leg pain that interferes with daily activities. It can lead to leg weakness or numbness and trouble with bowel and bladder control.
What can I do to prevent lumbar disk disease?
Maintaining a healthy weight, participating in regular exercise, and using good posture can lessen your risk for lumbar disk disease. Smoking increases the risk for disk herniation and should be stopped.
Living with lumbar disk disease
Conservative therapy requires patience. But sticking with your treatment plan can reduce back pain and minimize the chance of worsening pain or damage to the disk. Conservative measures and surgery can both take time to be effective.
When should I call my healthcare provider?
Call your healthcare provider right away if your pain increases or if you start having trouble with bowel or bladder control.
Key points about lumbar disk disease
-
Lumbar disk disease may occur when a disk in the low back area of the spine bulges or herniates from between the bony area of the spine.
-
Lumbar disk disease causes lower back pain and leg pain and weakness that is made worse by movement and activity.
-
The first step in treatment is to reduce pain and reduce the risk of further injury to the spine.
-
Surgery may be considered if the more conservative therapy fails.
Next steps
Tips to help you get the most from a visit to your healthcare provider:
-
Know the reason for your visit and what you want to happen.
-
Before your visit, write down questions you want answered.
-
Bring someone with you to help you ask questions and remember what your healthcare provider tells you.
-
At the visit, write down the name of a new diagnosis and any new medicines, treatments, or tests. Also write down any new instructions your provider gives you.
-
Know why a new medicine or treatment is prescribed and how it will help you. Also know what the side effects are and when they should be reported.
-
Ask if your condition can be treated in other ways.
-
Know why a test or procedure is recommended and what the results could mean.
-
Know what to expect if you do not take the medicine or have the test or procedure.
-
If you have a follow-up appointment, write down the date, time, and purpose for that visit.
-
Know how you can contact your healthcare provider if you have questions.