Status Epilepticus
What is status epilepticus?
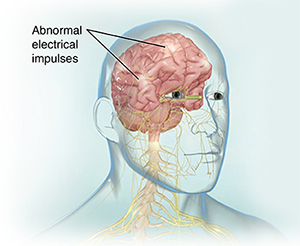
A seizure involves abnormal electrical activity in the brain. It affects both the mind and the body. Many problems can cause you to have a seizure. These include:
If you have epilepsy , you may have seizures again and again. You may have status epilepticus if you have a seizure that lasts longer than 5 minutes, or if you have more than one seizure without returning to a normal level of consciousness between episodes. This is a medical emergency. Call 911. It may lead to permanent brain damage or death.
Status epilepticus is very rare. Most people with epilepsy will never have it. This condition is more common in young children and elderly adults.
This condition can occur as:
-
Convulsive status epilepticus. This type occurs with convulsions. It may be more likely to lead to long-term injury. Convulsions may involve jerking motions, grunting sounds, drooling, and rapid eye movements.
-
Nonconvulsive status epilepticus. People with this type may appear confused or look like they're daydreaming. They may be unable to speak. They may also behave in an irrational way.
What causes status epilepticus?
In children, the main cause of status epilepticus is an infection with a fever. Children with severe, refractory seizure disorders can also have status epilepticus. In adults, the common causes are:
-
Stroke
-
Autoimmune disorders
-
Imbalance of substances in the blood, such as low blood sugar
-
Drinking too much alcohol or having alcohol withdrawal after previous heavy alcohol use
-
Withdrawal from medicines to treat seizures
Who is at risk for status epilepticus?
There are many risk factors for status epilepticus, such as:
-
Poorly controlled epilepsy
-
Low blood sugar
-
Stroke
-
Kidney failure
-
Liver failure
-
Encephalitis (swelling or inflammation of the brain)
-
HIV
-
Alcohol or drug abuse
-
Genetic diseases, such as Fragile X syndrome and Angelman syndrome
-
Head injuries
What are the symptoms of status epilepticus?
These are possible symptoms of status epilepticus:
How is status epilepticus diagnosed?
Your healthcare provider will do a physical exam. They will ask about your past health, any medicines you are taking, and if you’ve been using alcohol or other drugs.
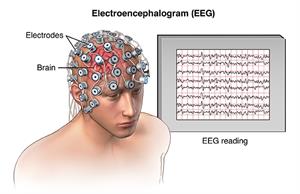
Your healthcare provider may also order an electroencephalogram. This involves placing painless electrodes onto your scalp to measure the brain's electrical activity.
 |
| PNerv_20140331_v0_001 |
You may need other tests to search for possible causes, such as:
How is status epilepticus treated?
The healthcare provider will want to end the seizure as quickly as possible and treat any underlying problems that are causing it. You may need:
Healthcare providers may also use antiseizure medicines to treat the problem, such as:
-
Diazepam
-
Lorazepam
-
Levetiracetam
-
Lacosamide
-
Phenytoin
-
Fosphenytoin
-
Phenobarbital
-
Valproate
These medicines are given through an IV or an injection into a muscle.
What are possible complications of status epilepticus?
Complications depend on the underlying cause. They can range from no problems to death. If the cause, such as poor epilepsy control, can be fixed, there may be no problems. If the cause is a stroke or brain injury, a person may suffer physical disability to even death.
Can status epilepticus be prevented?
If you have epilepsy, taking your medicines as directed may help you prevent this problem. If you’ve had status epilepticus, you may need to begin taking seizure medicines or change the seizure medicines you’re already taking. Keep a seizure log. Contact your provider if your seizures change in how often they happen, how long they last, or the type you’re having.
You may also be able to prevent this health problem by:
Key points about status epilepticus
-
Status epilepticus has many causes. Some can be prevented, such as low blood sugar or alcohol and drug abuse.
-
People who have epilepsy must take their medicine as told.
-
A seizure that lasts more than 5 minutes, or having more than one within a 5-minute period is an emergency. Call 911.
Next steps
Tips to help you get the most from a visit to your healthcare provider:
-
Know the reason for your visit and what you want to happen.
-
Before your visit, write down questions you want answered.
-
Bring someone with you to help you ask questions and remember what your provider tells you.
-
At the visit, write down the name of a new diagnosis, and any new medicines, treatments, or tests. Also write down any new instructions your provider gives you.
-
Know why a new medicine or treatment is prescribed, and how it will help you. Also know what the side effects are.
-
Ask if your condition can be treated in other ways.
-
Know why a test or procedure is recommended and what the results could mean.
-
Know what to expect if you do not take the medicine or have the test or procedure.
-
If you have a follow-up appointment, write down the date, time, and purpose for that visit.
-
Know how you can contact your healthcare provider if you have questions, especially after office hours or on weekends.