Knee Replacement Surgery
What is knee replacement surgery?
An artificial knee replacement may be considered when your knee is badly damaged by disease or injury, an artificial knee replacement may be considered. Your joint surfaces are replaced by prostheses during knee replacement surgery. These are plastic and metal parts that are used to replace your joint surfaces.
Why might I need knee replacement surgery?
Osteoarthritis is the most common problem that leads to knee replacement surgery. This is a “wear and tear” joint disease that affects mostly middle-aged and older adults. Osteoarthritis leads to the breakdown of joint cartilage, and then bone, in your knees.
Other forms of arthritis can also lead to degeneration of your knee joint. These include rheumatoid arthritis and arthritis caused by a knee injury. Breaks (fractures), torn cartilage, or torn ligaments also can lead to permanent damage to your knee joint over time.
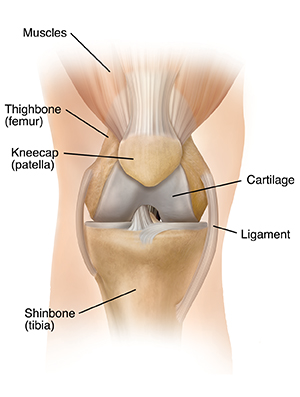 |
| Normal knee joint. |
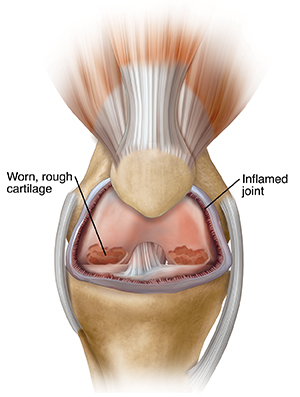 |
| Knee with arthritis. |
The decision to replace the painful knee with an artificial one is a joint decision between you and your healthcare provider. Other treatments may be used first. These include lubricating injections, steroid injections, physical therapy, assistive walking devices, and anti-inflammatory medicines that help with pain and swelling.
What are the risks of knee replacement surgery?
As with most surgeries, knee replacement surgery has risks. General anesthesia is used to put you into a deep sleep during surgery. Anesthesia poses risks for some people. Other possible risks include:
Long-term risks are not common, but can include:
There may be other risks. This depends on your specific health condition. Talk about any concerns with your surgeon before the procedure.
How do I get ready for knee replacement surgery?
Your surgeon will do a complete physical exam in addition to taking a complete health history . They may also take X-rays, urine tests, and blood tests to check your overall health before surgery. You may also meet with a physical therapist to discuss rehabilitation after the surgery, equipment you may need (such as crutches or a walker), and changes needed at home. These may include toilet seat risers, tub or shower safety bars, and secure handrails at stairs.
While the chance for infection after knee replacement is very low, it can occur. You may be asked to see your dentist before surgery. This is so that any major dental procedures you might need (such as tooth extractions and periodontal work) can be done before your total knee replacement surgery. This helps reduce your risk for infection.
Tell your surgeon about all prescription and over-the-counter medicines and any vitamins, herbs, and supplements that you are taking. Some of these may affect things like healing and blood clotting. You may need to stop taking them before surgery.
Follow any directions you're given for not eating or drinking before the surgery. You'll likely have to stay in the hospital for a few days. And you won't be allowed to drive for some time after surgery. You'll likely need some help at home (with things like bathing, dressing, cleaning, and shopping) for a short time after surgery. So you may want to arrange this ahead of time.
Talk with your surgeon so you know exactly what you need to do before your procedure.
What happens during knee replacement surgery?
Although each procedure varies, generally, surgery to replace your knee lasts about two hours. You may be under general anesthesia during surgery. This is medicine that puts you to sleep and keeps you from feeling pain during the surgery. The anesthesiologist may also give you a nerve block, or spinal or epidural anesthesia. These numb the lower half of your body so you don’t feel pain. You can remain awake with these medicines.
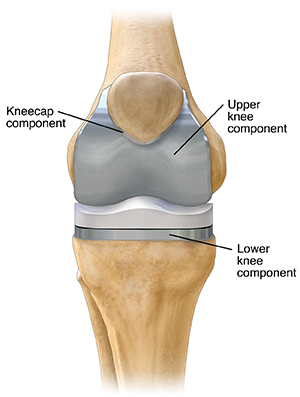
Your orthopedic surgeon will put your new artificial knee in place after the damaged bone and cartilage of your knee are removed.
The two most common types of knee prostheses used in knee replacement surgeries are cemented prosthesis and uncemented prosthesis. Sometimes a combination of the two types is used. A knee prosthesis is made up of metal and ceramic or plastic. A cemented prosthesis is attached to the bone with a type of epoxy. An uncemented prosthesis attaches to the bone with a fine mesh of holes on the surface. The bone grows into the mesh and attaches to the prosthesis.
The prosthesis (artificial knee) is made up of these three components:
-
Tibial component. This replaces the top of your shin bone (tibia).
-
Femoral component. This replaces your two thighbone (femoral) condyles and the patella groove.
-
Patellar component. This replaces the bottom surface of the kneecap that rubs against your thighbone.
What happens after knee replacement surgery?
After knee replacement surgery, you likely will go home the same day. Some people may have to stay in the hospital for one or more days. You will likely begin physical therapy exercises to start regaining range of motion in your knee soon after surgery. Your surgeon will work with you to reduce your pain and help keep you comfortable. Pain medicine and other pain management methods may be used. Pain management is important, because you need to start moving as soon as possible after surgery.
Your surgeon may also have you do things to help prevent blood clots and decrease swelling. For instance, you may wear special support hose, use compression boots (inflatable leg coverings) when in bed, and take blood thinners. You may also be asked to move your foot and ankle right after surgery. This is to increase blood flow in your leg muscles and help prevent swelling and blood clots.
You may be asked to take deep breaths or use a breathing tool called a spirometer to help prevent pneumonia.
The cut (incision) will have stitches or staples that will be removed after 1 to 2 weeks. Make sure you know how to care for this wound and keep it dry while it heals.
The recovery period can take a few months. In the meantime, you may need to adjust job duties. Or even take time off from work while you heal. You may need extra help at home and need to be especially careful not to fall and damage your new knee. Your healthcare provider will talk to you about activity restrictions and exercise plans you should follow after surgery.
Let your surgeon know about any of these:
-
Fever or chills
-
Redness, swelling, bleeding, or other drainage from the incision
-
Increased pain in the knee or around the incision
These problems may need to be treated. Talk with your surgeon about what you should expect. And when you should see your healthcare provider right away.
Long-term outlook
-
You should be able to straighten your leg and bend it well enough to climb stairs and get into a car.
-
It’s normal to feel or hear clicking in your new knee.
-
The incision may feel numb or stiff, especially when bending your knee.
-
Your prosthesis may set off metal detectors. Tell security agents about your knee replacement.
-
You will need to see your surgeon from time to time for follow-up exams and X-rays, often once a year.
-
Make sure your dentist knows about your knee replacement. You may need to take antibiotics before dental procedures.
Next steps
Before you agree to the test or procedure make sure you know:
-
The name of the test or procedure
-
The reason you are having the test or procedure
-
What results to expect and what they mean
-
The risks and benefits of the test or procedure
-
What the possible side effects or complications are
-
When and where you are to have the test or procedure
-
Who will do the test or procedure and what that person’s qualifications are
-
What would happen if you did not have the test or procedure
-
Any alternative tests or procedures to think about
-
When and how you will get the results
-
Who to call after the test or procedure if you have questions or problems
-
How much you will have to pay for the test or procedure